When it comes to matters of the heart, there’s perhaps nothing more fundamental than its rhythm. A regular, rhythmic heartbeat is a sign of a healthy heart, pumping oxygen-rich blood efficiently throughout the body. However, when this rhythm goes awry, it can spell trouble. One such cardiac irregularity is Atrial Fibrillation, often referred to as AFib.
In this blog, we’ll demystify atrial fibrillation, explaining what it is, how it occurs, and why it matters. We’ll dive into the mechanics of abnormal electrical impulses within the atria, leading to erratic heart rhythms. We’ll also illustrate the various types of AFib and its potential consequences on heart health and one’s overall well-being.
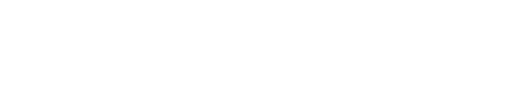
Understanding the Heart’s Electrical System
Before delving into Atrial Fibrillation, it’s essential to grasp the heart’s electrical system. The heart is not just a muscular pump; it’s also an intricately wired electrical machine. It has its own electrical power board, which controls the rhythm and coordination of the heart’s contractions.
The heart’s electrical system comprises several key components:
Sinoatrial (SA) Node: Often called the “natural pacemaker” of the heart, the SA node generates electrical impulses that initiate each heartbeat.
- Atria: The two upper chambers of the heart, known as the atria, receive blood from the body and the lungs. When the SA node sends an electrical signal, the atria contract, pushing blood into the lower chambers, the ventricles.
- Atrioventricular (AV) Node: This node acts as a gateway between the atria and ventricles, ensuring that electrical impulses pass from the atria to the ventricles at the right time.
- Ventricles: The lower chambers of the heart, the ventricles, receive the electrical impulses from the AV node and contract to pump blood to the rest of the body.
Normally, this system works harmoniously, resulting in a steady, regular heartbeat.
The Disruption of Atrial Fibrillation

Atrial Fibrillation, or AFib, occurs when there is a disruption in the electrical system of the heart, specifically in the atria. Instead of the SA node sending out a single, organized electrical signal, the atria quiver chaotically. These rapid and irregular electrical impulses cause the atria to contract in a disorganized manner. As a result, blood isn’t pumped effectively into the ventricles.
The chaotic electrical activity in the atria can lead to a fast and irregular heartbeat. In essence, the atria are no longer contributing to the effective pumping of blood, and the ventricles must compensate. This can lead to palpitations, shortness of breath, weakness, and fatigue.
Types of Atrial Fibrillation

Atrial Fibrillation isn’t a one-size-fits-all condition. It can manifest in several different ways, categorized into various types:
- Paroxysmal AFib: This type comes and goes. The irregular heart rhythm can last for a few seconds to a few days and then returns to a normal rhythm.
- Persistent AFib: In this case, the irregular rhythm lasts for more than seven days and typically requires treatment to restore a regular rhythm.
- Long-standing Persistent AFib: When the irregular rhythm persists for more than a year, it’s classified as long-standing persistent Atrial Fibrillation. Like persistent AFib, it often requires medical intervention to return to normal rhythm.
- Permanent AFib: In permanent AFib, attempts to restore a regular rhythm have failed, and the irregular rhythm becomes a constant feature. However, the heart is still treated to control the heart rate and reduce risk of complication.
Why Atrial Fibrillation Matters
Understanding Atrial Fibrillation’s impact on heart health and individual well-being is crucial. Here’s why it matters:
Blood Clot Formation: When the atria don’t contract effectively, blood can pool in the chambers. This stagnant blood is more prone to clotting. If a clot dislodges and travels to the brain, it can cause a stroke, which is a severe and life-altering event.
- Heart Failure: Over time, Atrial Fibrillation can weaken the heart muscle, leading to heart failure. The heart may not pump blood effectively, causing symptoms like shortness of breath, swelling in the legs, and fatigue.
- Increased Risk of Stroke: Atrial Fibrillation significantly increases the risk of stroke. In fact, it’s estimated that individuals with AFib are five times more likely to have a stroke.
- Reduced Quality of Life: The symptoms of Atrial Fibrillation, such as palpitations and fatigue, can significantly reduce an individual’s quality of life. Activities they once enjoyed may become challenging, and the constant worry about stroke risk can lead to anxiety.
- Other Health Complications: Atrial Fibrillation can lead to other health complications, including heart attacks, kidney problems, and even dementia due to reduced blood flow to the brain.
Diagnosis and Management

Diagnosing Atrial Fibrillation typically involves an electrocardiogram (ECG or EKG) or other monitoring devices that can detect irregular heart rhythms. Once diagnosed, the management of AFib aims to achieve two primary goals:
- Rate Control: This involves medications or procedures to keep the heart rate within a normal range, even if the rhythm remains irregular. This helps improve symptoms and reduce the risk of complications.
- Rhythm Control: Some patients may undergo procedures like cardioversion or catheter ablation to restore a normal heart rhythm. This can be more challenging, especially if Atrial Fibrillation has been present for a long time.
In addition to medical treatments, lifestyle changes play a crucial role in managing Atrial Fibrillation. These include:
- Medication Adherence: Taking prescribed medications consistently.
- Healthy Diet: Adopting a heart-healthy diet low in salt and saturated fats.
- Exercise: Engaging in regular, moderate exercise as recommended by a healthcare provider.
- Stress Management: Reducing stress through relaxation techniques like meditation, yoga, or even Tai Chi.
- Limiting Alcohol and Caffeine: These substances quicken the heart rate and can trigger Atrial Fibrillation episodes in some individuals.
- Quitting Smoking: Smoking is a risk factor for heart disease and can exacerbate Atrial Fibrillation.
The Bottom Line

Atrial Fibrillation may seem like a complex medical condition, but at its core, it’s a disruption in the heart’s electrical system that can have significant consequences for your health and well-being. Understanding its basics, including the types, potential complications, and management strategies, is essential for anyone affected by AFib or concerned about their heart health.
If you suspect you may have Atrial Fibrillation or have been diagnosed with it, working closely with your healthcare provider to develop a tailored treatment plan is crucial. With the right approach, many individuals with AFib can effectively manage their condition and lead fulfilling lives, prioritizing heart health and overall well-being. Remember, knowledge and proactive care are your allies in the fight against Atrial Fibrillation.